The Science Behind Poly-L-lactic Acid: A Biostimulatory Approach to Rejuvenation
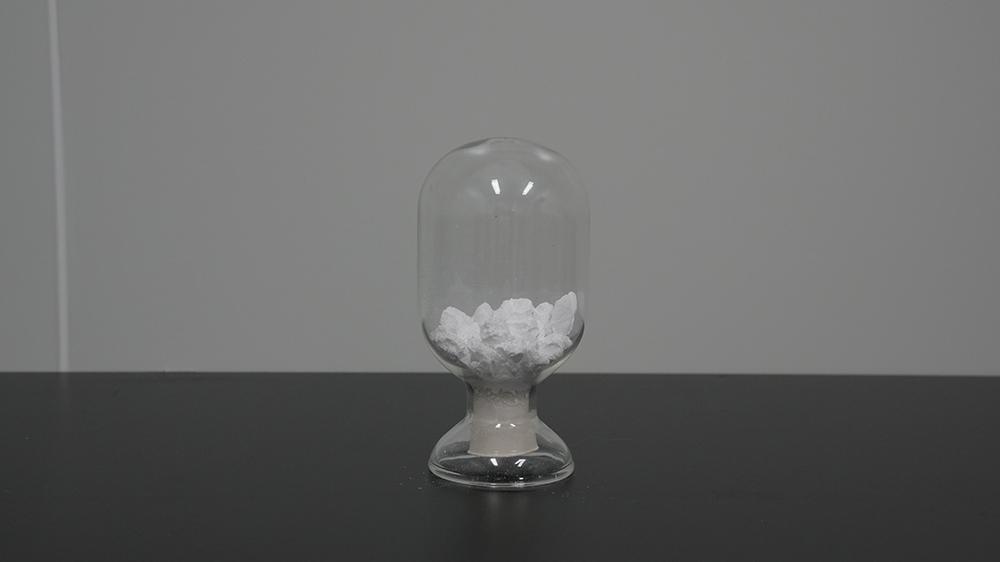
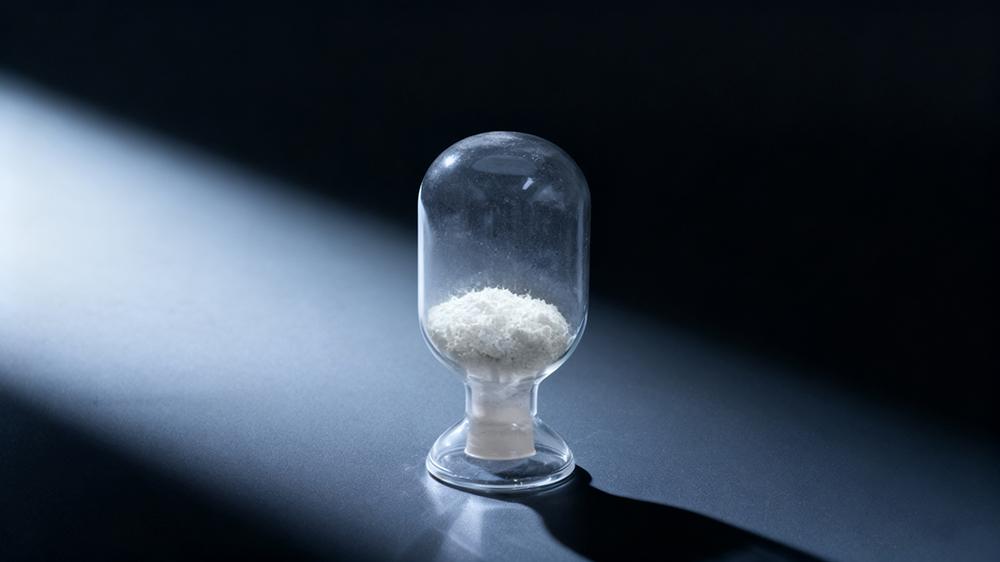
Poly-L-lactic acid (PLLA) is a bioabsorbable and biocompatible synthetic polymer widely used in aesthetic medicine and tissue repair. It was initially developed as a degradable suture material and has now become an FDA-approved injectable implant for facial volume restoration and wrinkle correction. The uniqueness of PLLA lies in its ability to gradually stimulate collagen production, allowing for long-lasting tissue repair and rejuvenation while maintaining a natural appearance.
I. Medical Applications of Poly-L-lactic Acid
The FDA first approved PLLA for the treatment of facial lipoatrophy (fat loss) in HIV-infected patients caused by antiretroviral therapy. Such patients experience significant facial fat loss, which affects both appearance and psychological well-being. PLLA injections can effectively restore facial volume and improve contours.
Subsequently, PLLA’s use expanded to immunocompetent individuals for the correction of nasolabial folds, wrinkles, and skin laxity associated with aging. Owing to its excellent biocompatibility and controlled resorption, PLLA is also widely used off-label for volume enhancement in areas such as the cheeks, temples, jawline, hands, neck, thighs, and buttocks. In reconstructive surgery, it has been used to assist in correcting chest wall deformities — such as pectus excavatum or postoperative chest asymmetry — and to improve contour irregularities following mastectomy or breast implant reconstruction.

In recent years, with advances in material science, companies like eSUNMed, which specialize in the synthesis and modification of biomedical polymers, have made continuous innovations in the preparation of PLLA polymers and PLLA microspheres, providing more stable and controllable medical-grade materials for clinical use. These technological improvements have enhanced the precision and safety of PLLA in regenerative medicine and tissue repair.
Researchers are also exploring the potential of PLLA in neural and bone tissue regeneration. For example, combining PLLA with polycaprolactone (PCL) to create repair patches for myelomeningocele (MMC) has shown the ability to maintain structural support while allowing controlled degradation — offering new possibilities for regenerative medicine.
II. Mechanism of Action
The long-term volumizing effect of PLLA injections does not result from the material’s bulk itself but from its biostimulatory action, which induces the body’s own collagen production.
The early post-injection volume increase is mainly due to the water content of the injection suspension and mild tissue swelling, which typically resolves within a few days. Subsequently, PLLA microparticles are phagocytosed by macrophages, triggering a mild and controlled inflammatory response. The particles gradually hydrolyze into lactic acid monomers, which are ultimately metabolized into carbon dioxide and water. During this process, fibroblasts are activated, promoting the sustained synthesis of type I collagen, which thickens and tightens the dermal and subdermal tissues.

The rejuvenation process usually becomes noticeable four to eight weeks after treatment and may last 12 to 24 months. About half of the PLLA material is absorbed within six months, while the newly formed collagen fibers continue to provide structural support, giving the treated areas a naturally fuller and more youthful appearance.
III. Safety and Adverse Reactions
PLLA is generally considered safe. As a biodegradable and non-immunogenic material, it is metabolized by the body without leaving any residual foreign matter. Common mild side effects include redness, tenderness, small nodules, or temporary asymmetry at the injection site, most of which resolve spontaneously. If the injection technique is improper or post-treatment massage is insufficient, more persistent nodules or fibrosis may occur.
Therefore, standardized procedures, adequate dilution, and appropriate post-treatment massage are essential to ensure both safety and effectiveness. The treatment should be administered only by properly trained medical professionals, avoiding superficial injections or excessive doses.
IV. Multidisciplinary Management and Clinical Significance
The success of PLLA treatment depends not only on the physician’s injection technique but also on multidisciplinary collaboration among dermatologists, plastic surgeons, nurses, and patients. From pre-treatment assessment and treatment planning to post-treatment monitoring and follow-up, the involvement of a professional team enhances both outcomes and safety.
The core value of PLLA lies in stimulating the body’s self-repair mechanism. Through a gentle biodegradation process, it promotes tissue regeneration, achieving natural, gradual, and long-lasting rejuvenation and structural remodeling.
Conclusion
The primary function of poly-L-lactic acid is to activate the body’s intrinsic regenerative ability by stimulating collagen production, thereby achieving skin rejuvenation and tissue remodeling. With its biodegradability, biocompatibility, and long-lasting effects, PLLA has become an essential material in modern aesthetic medicine and tissue engineering.
As domestic research in biomedical polymers continues to advance, companies such as eSUNMed, which focus on the development of biomedical polymers, are providing higher-quality and locally manufactured PLLA materials. This progress supports safer and more effective clinical use of PLLA, broadening its prospects in both medical aesthetics and regenerative medicine.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Juegos
- Gardening
- Health
- Inicio
- Literature
- Music
- Networking
- Otro
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness


