Revitalizing Urgent Care Revenue Cycle Management with ASP-RCM Solutions
Urgent care centers face heavy patient flow, strict clinical documentation needs, and fast turnaround expectations. Because of this, accurate urgent care billing, powerful workflow systems, and clean claim submission are essential for stable revenue. Many clinics struggle with denied claims, wrong coding usage, and slow payments, which directly hit financial performance. A strong approach to Urgent Care RCM helps providers maintain efficiency, deliver quality care, and secure predictable cash flow.
Why Urgent Care Billing Is Complex
Urgent care billing operates differently from primary care or specialty clinics. Visits involve unscheduled patients, diverse treatments, and rapid documentation. Each encounter must be coded correctly using urgent care CPT coding so payers accept claims without objections. Errors in modifiers, POS codes, or evaluation levels result in revenue loss. To avoid this, clinics depend on structured urgent care billing services designed for high-traffic environments.
Key Components of Effective Urgent Care RCM
1. Accurate Patient Registration
Correct demographic entry is the first step in Urgent Care Revenue Cycle Management. Small mistakes like wrong DOB, insurance ID, or payer information create claim rejection. A streamlined registration workflow supports clean claim creation.
2. Real-Time Insurance Verification
Insurance eligibility must be verified before treatment. Without accurate verification, clinics face payment delays. Automated verification solutions used inside urgent care billing services help staff confirm coverage instantly.
3. Detailed Clinical Documentation
Every urgent care visit requires complete chart notes. Missing clinical details affect urgent care CPT coding accuracy. For example, procedures, injections, X-rays, and wound repairs must be recorded clearly so coders select correct CPT codes for billing.
4. Correct Coding With Urgent Care CPT Coding
Coding is a major pillar of Urgent Care RCM. Coders must apply exact CPT codes for:
-
E/M levels
-
Diagnostic services
-
Minor procedures
-
Lab tests
Correct usage of modifiers improves reimbursement. Regular coding audits inside urgent care billing services increase compliance and reduce payer issues.
5. Charge Entry & Claim Creation
Once coding is completed, charges are posted into the billing system. Claims must be created with accurate service details. Any mismatch between coding, documentation, or payer rules causes denials.
6. Timely Claim Submission
Urgent care billing must follow strict payer timelines. Late submission lowers acceptance rates. Automated claim submission improves speed and reduces human errors.
7. Denial Management
Denied claims must be analyzed and corrected immediately. Common denial causes include lack of documentation, wrong urgent care CPT coding, or insurance mismatch. A robust denial management cycle increases recovery rate inside Urgent Care RCM.
8. Payment Posting
Payments from payers must be posted without delay. Discrepancies must be resolved quickly to avoid future claim conflicts. Posting accuracy gives a realistic view of clinic performance.
9. Reporting & Analytics
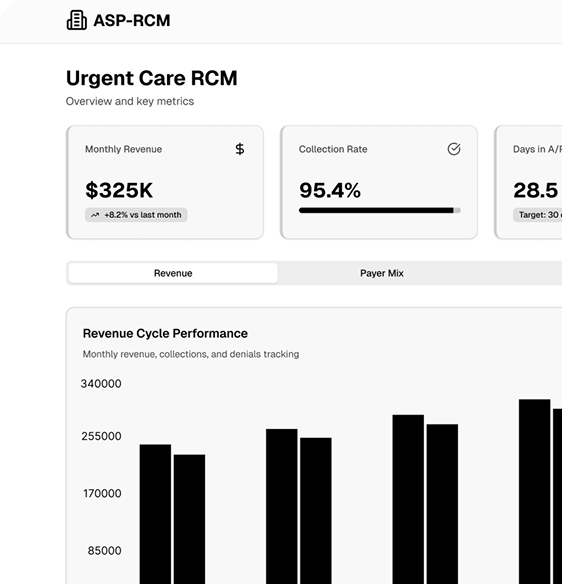
Urgent care billing services include detailed KPI tracking such as:
-
Days in A/R
-
Denial rate
-
Clean claim rate
-
Collection percentage
These insights highlight where financial improvement is required.
How Urgent Care Billing Services Benefit Clinics
✔ Faster Payments
Optimized urgent care billing workflows reduce errors and speed up claim approval.
✔ Reduced Administrative Pressure
Outsourced urgent care billing services allow staff to focus on patient care.
✔ Higher Clean Claim Rate
Correct CPT coding, proper documentation, and real-time verification reduce rejection volume.
✔ Better Revenue Stability
Efficient Urgent Care RCM ensures consistent monthly income.
Revenue Cycle Strategies That Improve Performance
1. Standardized Workflow
Consistent documentation templates and coding guidelines make urgent care billing smoother.
2. CPT Coding Updates
Urgent care CPT coding is revised regularly. Clinics must stay updated with annual changes.
3. Staff Training
Front desk, billers, and coders need training on patient intake, insurance rules, and payer-specific guidelines.
4. Technology Adoption
Using automated RCM software, AI-based coding tools, and electronic claim submission increases productivity inside Urgent Care Revenue Cycle Management.
5. Compliance Checks
Regular internal audits reduce compliance risks and ensure that claims meet payer policies.
Future Trends in Urgent Care RCM
Urgent care centers are adopting AI-powered coding, predictive analytics, and real-time denial prediction systems. These technologies minimize manual work and increase billing speed. Integrating EHR with billing platforms creates seamless data flow that supports accurate CPT coding and faster reimbursement.
Conclusion
Urgent care billing requires precision, updated CPT coding knowledge, strong claim management, and consistent workflow monitoring. With professional urgent care billing services, clinics achieve smoother operations and stronger revenue. A well-structured Urgent Care RCM framework supports accurate documentation, compliant coding, faster claim submission, and improved cash flow.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Παιχνίδια
- Gardening
- Health
- Κεντρική Σελίδα
- Literature
- Music
- Networking
- άλλο
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness


