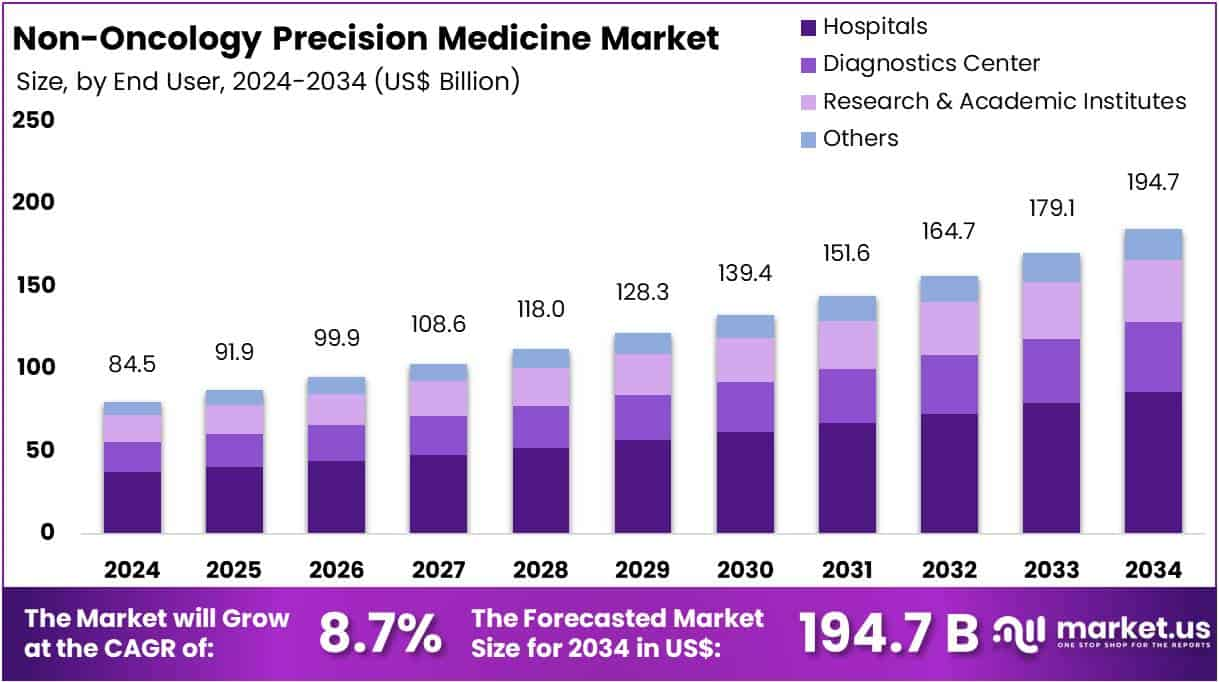
The Global Non-Oncology Precision Medicine Market is projected to reach around US$ 194.7 Billion by 2034, up from US$ 84.5 Billion in 2024. It is growing at a CAGR of 8.7% from 2025 to 2034. North America currently leads the market, holding over 44.2% share, valued at US$ 37.3 Billion. This growth reflects rising demand for personalized treatments in non-cancer areas. Key segments include cardiovascular, metabolic, and autoimmune diseases, with innovation and data-driven approaches playing a central role.
Government support is accelerating non-oncology precision medicine development. In the U.S., the Precision Medicine Initiative is broadening its focus to chronic illnesses beyond cancer. It emphasizes data collection from genetics, environment, and lifestyle to enable individualized care. The aim is to create scalable databases for treatment insights. This foundational support builds long-term infrastructure. Areas like diabetes and heart disease are benefiting. Such initiatives ensure sustained growth for personalized healthcare by improving access and boosting research-backed solutions.
Europe is also making significant strides through the Horizon Europe program. The initiative funds personalized medicine research, especially for neurodegenerative diseases such as Alzheimer’s. By supporting clinical trials and cross-border data sharing, it enhances collaboration across EU nations. These programs are helping deliver more evidence-based and patient-specific treatments. Europe is positioning itself as a leader in precision diagnostics. Continued investment in R&D and multinational projects enhances innovation and market competitiveness in non-oncology areas.
Public health and precision care goals are aligning globally. Governments are promoting partnerships among research institutions, biotech firms, and healthcare providers. These collaborations foster improved access to diagnostics and reduce treatment inconsistencies. Increased funding is expanding pipelines for new therapies. Autoimmune and endocrine diseases are among the first to benefit from these innovations. Regulatory frameworks are also evolving to support clinical integration. As adoption rises, non-oncology precision medicine is becoming a key pillar in next-generation healthcare systems.
Polygenic Risk Scores (PRS) are reshaping non-oncology precision medicine. PRS assess genetic risk across various markers to predict disease likelihood. They are being applied to cardiometabolic conditions like coronary artery disease and type 2 diabetes. PRS enhances early detection and risk profiling, shifting healthcare from reactive to proactive. Clinicians use PRS to better categorize patients based on genetic risk. This approach enables early interventions, targeted screening, and personalized prevention strategies. As data access improves, PRS is set to play a major role in future precision care models.